Colombia, a country at war for over fifty years, has one of the highest rates of landmine injuries in the world. For decades, landmine victims have remained outside the nation's popular consciousness. Today, landmines and rehabilitative medicine profoundly shape public life. This article shows how the seemingly mundane activity of walking becomes a strangely familiar experience among amputees and an increasingly technical one among medical practitioners in Colombian rehab units. It's worth noting that when patients and medical staff discussed how they or their patients learned how to walk using prostheses, they also often talked about their experiences with phantom limbs. As subjective as bodily sensations are I argue that they are nonetheless implicated in social relations of power and political and economic change. Within rehab medicine, clinicians frequently see phantoms as part of a patient's healing process and sometimes worry that failing to experience the amputated limb as a felt presence makes recovery more difficult. Without a missing object, there is no object to desire, they presume. Rather than treat phantom limb sensation as a kind of psychosis, this essay explores how the Colombian medical establishment talks about rehabilitation with prostheses as a form of social, physical, and psychological integration. I also show how patients, meanwhile, experience a kind of ambivalence—marked by oscillating feelings of strangeness and naturalness—regarding limb loss and the prostheses they use to manage it.
Introduction
Colombia, a country at civil war for over fifty years, has one of the highest rates of landmine injury in the world. While for decades landmine victims remained outside the nation's popular consciousness, landmines and rehabilitation medicine now profoundly shape public life. This essay, based on more than four years of ethnographic research in a military hospital, a military battalion, and a civilian charity home in Bogotá, Colombia, explores how the seemingly mundane activity of walking becomes strangely familiar among amputees and increasingly technical among medical practitioners in Colombian rehab units. Yet, when patients discuss how they learned to walk using prostheses—or when medical staff explain what it's like to help people learn this vital skill—they often refer to the pervasive experience of phantom limbs. Though bodily sensations are by definition subjective, I argue that such dynamics are implicated in social relations of power and political and economic transformation.
This essay explores questions of embodiment in relation to how people incorporate prostheses into their bodies. In 1938, French sociologist Marcel Mauss described the human "person" as inseparable from his or her bodily awareness. For Mauss, the construct of the "person" shared resemblances to "primitive" ritual masks where people wore a mask and performed a specific role, or persona. Mauss suggested that the individual is both an individual self and a social person who performs a role in society. 1 If embodiment, as Mauss suggests, is central to the way the "person" is constructed, what happens when a person's body changes dramatically?
Fragmentation, Integration
Colombia is said to be one of the oldest democracies in Latin America, yet it stands out as, arguably, the most politically divided nation in the Americas. Government military forces, paramilitary groups, and armed guerillas fight each other against the backdrop of an illicit narcotics trade. For a nation wracked by sectarian violence, "integration" of the physical body evokes dreams of a more integrated body politic — one that instantiates peace, cohesiveness, and enhanced social status among its citizenry. A current focus on "integration" imagines the body as comprised of parts and elements that are assembled in ways that enhance human capacity and expand corporate development in Colombia. As you will soon read, Colombian medical staff compare prosthetic body parts and their attributes to different brands of cars. Likewise, prosthetic users stylize their prosthetic limbs by ingeniously realigning parts and decorating them. This view is in marked contrast to the ways war torn bodies were portrayed during La Violencia (1948-1954), Colombia's bloodiest civil war, when Colombian nationals commonly depicted the human body as dismembered and rearranged. During La Violencia, Liberals as well as Conservatives argued over how boundaries between the church, the Colombian nation-state, and national territory should be drawn. In this war, combatants shot their victims in the head, cut up their bodies with machetes and displayed human remains in macabre configurations—such as tongues pulled through slit open throats and severed limbs inserted into torsos. 2 What belonged inside the body was placed outside of it and what belonged outside it was stuffed back in. Rumors about mutilated bodies spread like wildfire throughout Colombia's countryside. While today's focus on "integration" is a positive development, it is also elusive. "Integrated" rehabilitation underscores the continual violence inflicted on Colombian citizenry while also referring ironically to processes that attempt to unify the physical body and the nation-state.
My discussion focuses on men's bodies, consistent with the overwhelming majority of soldiers and civilians I encountered. Many men who have lost limbs by landmines were miners and farmers for whom becoming a military soldier represents an elevation of social status. Soldiers value limb loss as evidence of their sacrifice. On the other hand, people experience amputation as shameful because it explains how they lost their jobs as soldiers and how they were demoted to civilian status. Even more distressing, civilians injured by landmines risk being confused as an enemy by both guerilla and military forces. The categories of civilian and soldier are especially contentious in an environment where human rights discourse and Catholic notions of sacrifice are both operative. Amputation also compromises both civilian and soldier amputees' status as men within the domestic division of labor as they felt less able to obtain a job and provide for their families.
Within rehab medicine, clinicians often see phantoms as a gauge for a person's ability to incorporate prosthesis successfully. They believe that if the patient fails to sense the presence of the amputated limb, s/he will reject the prosthesis because s/he will not intuitively perceive something missing. Without a missing object, there is no object to desire. Taking this clinical attitude as my intellectual point of departure, this article examines how phantom limb sensation went from being a symptom of psychosis to a highly valued entity in Colombia and beyond. It will explore how the Colombian medical establishment considers rehabilitation with prostheses as a form of social, physical, and psychological integration. Patients, in contrast, express a kind of ambivalence—defined by oscillating feelings of strangeness and naturalness—towards their prostheses and their limb loss. Patients speak about prostheses not in terms of 'integration' but in terms of how prostheses made them look.
It is crucial to explore the phenomenological aspects of these processes since prosthetic incorporations call attention to the limits and boundaries of our bodies and the broader contexts to which they are connected. Prostheses are manufactured products that are aligned in such a way that they reflect how people create social order, how they imagine their worlds. Prostheses provide a window into understanding how cultural objects become incorporated into the body and the self and ultimately how they transform how people understand the body as a political, social, and personal entity. The way people wear prostheses leads them to diverse social roles. For this reason, it is crucial to consider how individuals incorporate cultural forms and values that they come to call their own—how people make their bodily performances intelligible to others—to note the moments when cultural performances register a disconnect between the person and the body in ways that motivate social change or invite critical reflections on the world.
In ethnographic interviews, people who had lost limbs discussed prostheses as simultaneously strange and familiar parts incorporated into their bodies. I knew Jhon Luis, a nineteen-year-old soldier, during his entire stay at Bogotá's Military Hospital—from the day the surgical staff told him that they would need to amputate his leg. Subsequently, he waited more than three months for his prosthesis. Not surprisingly, he got bored of waiting. He wanted to learn how to walk so he could leave the military health battalion, live with his girlfriend and visit his mother. When he finally received news that his prosthetic limb had arrived at the hospital and his leg was being assembled, he was elated. Jhon invited me to the hospital to share this exciting moment.
The first time Jhon put on his prosthesis, he gasped—eyes opened wide as if he was experiencing an electric shock, "It feels strange, really strange," he told me. Jhon tried to stand, and then walk, using the parallel bars. He did not fall and seemed to learn quickly, yet his face revealed how disconcerted he felt. Jhon Luis' new prosthesis seemed to transform something familiar like walking into something strange. After months of daily practice, Jhon could use his prosthesis so effortlessly that no one could tell he was wearing a prosthetic. His apparatus had by then become "second nature." With his new limb, Jhon walked in a way that we might compare to linguistic fluency. It was the kind of newly embodied sense of self that people frequently likened, at another level, to the struggles that Colombia's medical establishment had experienced.
Colombian Medicine in the post-War period
US wartime medicine has profoundly influenced Colombian military medicine since WWII. In 1946, Colombia drafted and passed law 90 for Obligatory Social Security (informed by the FDR's New Deal Social Security Act), which ensured federal funds towards public health. Law 90 promoted the creation of rehabilitative services in Colombian medicine and expanded services provided by the Central Military Hospital. The Central Military Hospital became a major Colombian establishment in the 1950s. In 1993, however, the State radically decentralized Colombia's public healthcare system by passing Law 100 for Integrated Social Security. Since then many state-funded public hospitals closed and medical worker unions collapsed. Law 100 effectively reverted state funds to private healthcare institutions.
In Colombia, state social services have declined and in their place the government has developed numerous training programs that make Colombian workers fit a corporate labor market. In free trade agreements, what is made 'free' is Colombian tariffs on US exports so US consumer goods become less costly to Colombian consumers; and, in effect, Colombians consume more US products. What US-based multinational corporations offer Colombia is employment and 'development' in exchange for cheap skilled Colombian labor. From the perspective of the US, investing in Colombia is seen as risky yet potentially lucrative. To secure foreign investment and diminish risks for multinationals, the Colombian state employs its military to acquire and protect territories so corporations can exploit petroleum and coal. In effect, farmers are forced to give up their land and livelihood. Many of these farmers flee to urban centers and are then regarded as 'displaced' persons. Indeed, Colombia is considered to have one of the largest internally displaced populations in the world, numbering approximately 4 million people. Through UN development programs for the displaced and USAID programs from landmine victims, war victims are funneled into 'integration' training programs to become low-level corporate laborers.
Farmers, however, are not the only ones losing territory and being deskilled. Medical professionals such as doctors, physical therapists, and prosthetists feel that they too are quickly being phased out. In partnership with humanitarian aid organizations, the centralized government is requiring Colombian medical institutions to meet international standards for rehabilitation, which include standard certification for specialists such as prosthetists and physical therapists. Hospitals and medical professionals are compelled to apply international standards to their practice in order to secure funding from USAID, the Japanese government, and other international funding sources. Policy makers, medical directors, corporations, and international health organizations continually try to standardize walking, or proper gait, both in patients' bodies and in the discourse of medical practice. International standards have become translated into specified forms of measurement that assure compliance to bureaucratically ascribed 'norms.' To enforce international standards, funding agencies and hospital administrators have turned to simulation technologies to calibrate gait by producing numerical data that records micromovements of the body within one "gait cycle." While some claim that simulation technologies allow physical therapists (PT's) to calibrate a patient's gait more accurately, seasoned physical therapists insist that they have developed alternative techniques that are more effective. I understand them to mean that simulation technologies do not capture the intuitive sense people have employed to successfully incorporate prostheses into their bodies. This intuitive sense involves phantom limb sensation.
Revaluing phantom limbs in and beyond the rehabilitation unit
Maria, the head physical therapist at the military hospital, explained that in the not-so-distant past, patients with amputations who reported phantom limb sensations would be admitted into the psychiatric ward in Bogotá. She explained that the military hospital now values phantom sensations and they are no longer seen as a symptom of 'psychosis.' According to Maria, when the patient feels like his foot, rather than the prosthesis, is touching the ground, he can more easily make any adjustments needed to perform a natural walk. Consciously, this may involve an adjustment in how he kicks out his prosthetic leg or swings his arms in rhythm with his feet. Eventually these movements become naturalized, or performed unconsciously. Maria trains patients to use phantom limbs as a way to perform what she calls 'biofeedback'. Neurologists use the term 'biofeedback' to refer to a looping effect between the brain and receptors throughout the body. However, phantoms and prostheses do not have nerve receptors. Obviously, in Maria's description of 'biofeedback,' the looping effect is present despite the absence of the flesh limb.
Maria also described a seemingly strange yet common phenomenon called 'telescopia' where people's phantom limbs shrink over time. It was not unheard of for an amputee to feel a phantom toe wiggling out from his knee. At other times, phantom limbs could be stretched or fragmented, so that a telescoped hand might, for example, reach out into space without an arm that connects it to other parts of the body. In 1872, American Civil War Surgeon Sir Silas Weir Mitchell wrote that "sensorial delusions" connected to people who have lost limbs "are so vivid, so strange" 3 it was curious that few of his colleagues found this topic worthy of study. In fact, he risked professional ridicule by acknowledging them as anything other than mere flights of reason.
Today neuroscientists are reviving scientific interest in what they have termed "telescopic phantom sensations." Colombian neuroscientist Rodolfo R. Llinas wrote a Colombian best seller El cerebro y el mito del yo 4 (translated into English as The I of the Vortex) where he argues that the self is a myth and that all humans live in a virtual reality generated through synaptic transmissions. Privileged with a prologue by Gabriel Garcia Marquez, this book was widely read and discussed in Colombia. In the United States, Dr. Ramachandran, author of Phantoms in the Brain, 5 has become a celebrity scientist for his ability to 'amputate' bothersome phantom limb sensations using what he calls a Virtual Reality Box consisting of an ingenious contraption of cardboard and mirrors. His Virtual Reality Box has been a feature story on National Public Radio and in the New York Times—it even made an appearance on an episode on the hit television show, House. The Virtual Reality Box is now being used around the globe as a cost-effective rehabilitation technique for people injured by landmines and other war explosives.
On one hand, the positive light now shining on phantom limbs opens a space for people to talk about experiences long dismissed as mere delusions. Moreover, as phantom limb sensations gain academic credibility, they have inspired innovative, cost-effective, and affective technologies like the Virtual Reality Box. On the other hand, it might also be worth asking how exactly scientists, medical professionals, and people more generally have shifted interest from the "whole" self to the phantasmagoric self, specifically one with the ability to telescope its parts and extend them out into space. Political and economic changes may account for some of the reasons we are encountering what may be a watershed moment in the way we have come to understand the self.
During my fieldwork, medical staff routinely complained that they felt they were losing control of their practice because corporations linked to humanitarian aid-funding inspired competition among medical institutions within the military. Unlike the hierarchical factory of the 1950's with worker drones and foremen, today's corporations aim to flatten hierarchies, downsize, and expand their spatial dimensions as they adapt to a changing market. 6 Corporations take dynamic, shapeshifting forms where workers are seen as replaceable. Likewise, people are expected to shapeshift, to constantly adapt to new modes of 'integration' in order to secure a livelihood. Living in a fiercely competitive world where securing resources for oneself has become much more difficult, people have shifted how they perceive time and space. Perhaps, this is one explanation about why the expanding and shrinking properties of telescopia have gained so much popular and scientific appeal.
Indeed, corporations are encouraging medical professionals to think virtually. Tomas, a Colombian designer living in Canada who works in the field of simulated medicine, told me that he created prototypes for Virtual Reality medical equipment, including those used for the Da Vinci Surgical System. To the novice, Da Vinci seems like a bizarre sci-fi contraption that requires a surgeon to peer through VR goggles, as s/he controls a robotic claw that performs surgery on a patient from a short distance. However, corporations are marketing Da Vinci and similar technologies such as PHANTOM® as the latest development in laparoscopic precision surgery using what is called 'phantom based haptic design'. While Da Vinci and PHANTOM® are advertised as precision instruments, designers do not actually possess the computational tools required for doctors to execute surgical procedures which require tactile feedback. For example, computational programs cannot code the fluid dynamics of blood or the squishiness of flesh in 3D real time, making it difficult for a surgeon to insert a needle into the patient's body without causing serious injury. Moreover, as Tomas explained to me, Da Vinci is a 20 million dollar piece of equipment, and thus too costly to use widely. On the flip side, designers see a future where the Da Vinci System will be more cost-effective, enabling US and Canadian doctors to conduct virtual surgery elsewhere—most notably in sites where the US military provides aid for war efforts, as medical professionals have noted they aspire to do.
The Da Vinci System has not yet arrived in Colombia; however, medical staff at the military hospital worry about the advent of telemedicine and its potential to devalue their embodied knowledge as practitioners. In the case of prosthetic limbs, telemedicine involves a computer system that will read a person's posture and residual limb. A single clinician will manage the computer system and send graphic and numerical information directly to a prosthetics company. The company will then customize a prosthesis based on this information and send it right to the user. In effect, telemedicine is seen as a threat, as a development likely to diminish the role that medical professionals currently play in rehabilitative care.
Acquiring Proper Gait In the Body
In the training room, physical therapists, comprised of young women, lead exercise routines every morning to salsa and pop music from the likes of Madonna and Eminem. Patients joke and tease, calling each other "mocho," or "cripple," and often tried to push each other down as physical therapists scold them. After exercise routines, the head physical therapist passes out forms for all the patients to sign that verifies their participation in rehabilitation for the day. Every Tuesday, a team of male orthopedic surgeons who perform amputations and follow-up observations enter the training room along with the prosthetists to evaluate patients' progress. This event is called "revisión" and it occurs once a week. As the surgeons enter, the jovial environment becomes quiet. If and when the group becomes rowdy, the surgeons demand silence. The doctors take various measurements of each patient's residual limb or limbs and then evaluate the alignment of his or her stance and the naturalness of his or her gait. Medical staff and patients sometimes joke, calling "revisión" "la pasarela" or catwalk. And indeed, the medical team asks them to walk across the room while they watch and discuss the performance. They even sometimes intercede, "You have to swing your arms a little. The rhythm of your walking must be continuous. Relax. Get some swing into it." Then, when the patient makes an adjustment, "No, that's a little too much" or "Yes, that's right…Isn't that better?"
The medical team observes without speaking very much. They each make gestures with their hands to indicate whether modular units are aligned correctly. The surgeon gives an eye signal to catch the attention of the PT (or prosthetist), tilting his hand to either the left or to the right. The prosthetist sometimes tells the patient to stop walking and, in the midst of an evaluation, he might use a monkey wrench to tighten or loosen the screws at the 'ankle', or what is referred to as the 'pyramid.' By adjusting the pyramid, the prosthetist can fine-tune the tilt of a foot. He can slightly tilt the foot in or out or change the foot's flexion in relation to the 'leg,' which medical staff refers to as the 'tube.'
The PT lifts the patient's shirt and feels with her hands whether the patient's hips are aligned. Then the staff asks the patient to start walking again. Meanwhile, observers provide input ("The right foot is tilted out…He's kicking out with his left foot too much"), although the surgeon always has the final say. Once he determines that the limb's alignment and gait are correct, the evaluation ceases and another patient is called up.
After this stage in the analysis called revisión, the team of surgeons leaves the room and the physical therapists recover all prosthetic limbs from the patients. Directing their displeasure to the young physical therapists, patients complain when their limbs are taken away. Many insist that they can not leave their residence at the military battalion or visit their families without them. Yet, hospital staff are firm that limbs can not leave the hospital until their owners have finished rehabilitation and doctors release the limbs.
At the military hospital, an orthopedic surgeon prescribes a prosthesis to each individual patient, much like a doctor prescribes pills. In his prescription, he specifies the weight, elements, and materials to be used in the patient's prosthesis. The surgeon takes into account the age, weight, and lifestyle of the patient. If a patient has lost one leg, then he traces the outline of the patient's other foot and includes this within the prescription so that a matching size foot can be selected for the patient's prosthesis. He also touches and feels the muscular articulations within the residual limb so that he can better recommend an appropriate exercise regimen in the prescription and to ensure that the prosthesis is properly fitted. The orthopedic surgeons at the military hospital explain to me that surgical techniques have not changed since they first became surgeons. Meanwhile, prosthetic design has changed dramatically, transforming the way they prescribe prostheses. In the past, prostheses were described as 'exoskeletal' since the prosthetist carved a whole prosthetic leg from one piece of wood. Today's prostheses are modular assemblages.
At the prosthetics workshop, the prosthetist adds ribbons of carbon and glass fibers to the limb socket to give it rigidity. They talk about how rotating knees and light titanium tubes are less stable than wooden limbs, but they are desirable since they increase flexibility and agility of the limb. As modular assemblages, prostheses can also be disassembled and rearranged. The medical staff at the military hospital first attempted to control prescriptions by only permitting each patient to own one prosthesis per missing part. If the patient needed a new limb, he would have to exchange his old one for the new prosthesis. However, the national landmine campaign in Colombia more recently opened the doors to a deluge of multinational corporations that specialize in prosthesis and international humanitarian organizations (sometimes a sub-branch of the corporation as in the instance of the Otto Bock Foundation) that donate limbs.
In Colombia, prosthetic companies market their products on the nightly news and on posters strategically placed throughout clinics and hospitals. While doctors and therapists recognize the benefits of the landmine campaign for improving rehabilitative care for soldiers, they also share complaints amongst themselves. They often talk about how humanitarian organizations donate limbs indiscriminately and how corporations market limbs in ways that exaggerate the benefits of costly prosthetic parts. It is not uncommon for both soldiers and civilian amputees to express their interest in prosthetic designs that are not accessible to them, or are too expensive. Soldiers often fantasize about costly prosthetic legs they watch being donated to Iraq Veterans in the U.S. on television.
Soldiers and physical therapists would frequently compare prostheses to automobiles. As Maria, the physical therapist I mentioned before, explained,
Prosthesis are like cars. There's a big range. You can have an Audi. You can also have a Renault Twingo. [The Twingo] will give you the same service, but is less expensive. We'd love to give our patients hydraulics with electronic and computerized parts, but this armed conflict is too big and if we give those prostheses to some then not everyone could have one.
The Twingo, which derives its name from "Twist", "Swing", and "Tango," was conceived by the French car company Renault as a simple, cost-effective car produced for Colombian markets in the 1990s. Thus, comparing cars and prostheses is not as far-fetched as it might at first seem, if only because Otto Bock produces both car parts and prostheses using the same materials for both.
While corporations set many parameters around prosthetic design, amputees find ways to make their own industrial limbs. Even though the hospital limits the number of limbs a patient can acquire, some soldiers manage to collect multiple limbs from humanitarian aid organizations. Treating limbs like cars, they customize their limbs by rearranging and interchanging their constituent elements. Through their exposure to corporate marketing, they know what parts are more costly and desirable. They also know how to assemble them in distinctive alignments. Soldiers mimic, and in some ways overturn, the prescriptive power of their surgeons, causing a great deal of frustration among doctors at the military hospital.
On the one hand, corporations and humanitarian aid fragment power relations. They open an opportunity for patients, who are treated as less powerful figures within the military, to participate in manipulating the objects they incorporate into their bodies. In this respect, corporations democratize Colombian medicine by displacing figures like military doctors, who embody and wield state authority. On the other hand, as I discussed above, corporations and humanitarian aid commodify healing, creating disparities of access to desired objects.
Gait Lab: 'to sit and analyze, you wonder why am I doing this'
Infrotex, an Austrian company, introduced Gait Lab to Colombia in April 2008 at Bogotá's Military Health Battalion. Gait Lab is a walking laboratory that uses video cameras and a computer program to record the various angles and positions of joint articulations that move during a person's gait cycle. As with most prosthetic-related technologies produced in Germany and Austria, the development of Gait Lab is based on research conducted within the United States. Former US army physical therapist and orthopedic surgeon, Jacqueline Perry, helped develop what is called Modern Gait Analysis, the conceptual base of Gait Lab. Perry describes a gait cycle as a single sequence where limbs alternate weight from one foot to another, propelling the body forward. According to gait analysis experts, the gait cycle consists of two time periods — stance and swing. Each time period is subdivided into intervals and varies in relation to gait velocity and body alignment. The table below shows the division of the gait cycle.
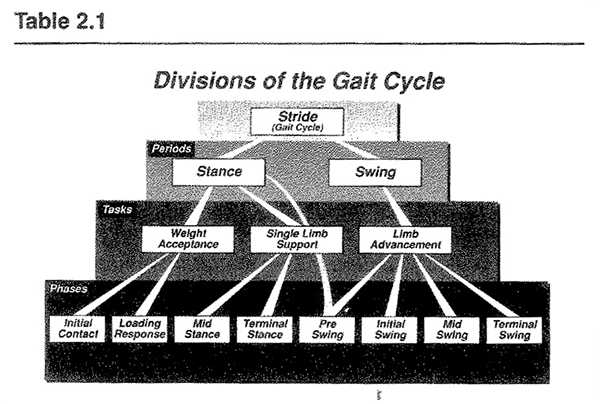
The intervals are divided into eight phases. Each of the eight phases is again subdivided into sequential combinations or 'functions.' Gait Lab engineers code the 'functions' of walking (or, in Perry's terminology, 'the locomotor system') in a computer program to create an 'integrated data system.' When a clinician measures a patient's walking with Gait Lab, it produces graphs, numbers and curves. Gait Lab provides a complex set of data compared against a norm, or medium, taken from a selection of 'normal' 'non-pathological' bipedal human walkers, represented by a stable curve on the graphs that Gait Lab computes. I began observing Gait Lab three months after its arrival at the health battalion in Bogotá. Linda, a young physical therapist at the battalion had started training with Gait Lab and was the first of her colleagues to do so. I would find her often studying Gait Lab graphs alongside a copy of Jacqueline Perry's textbook, Gait Analysis.
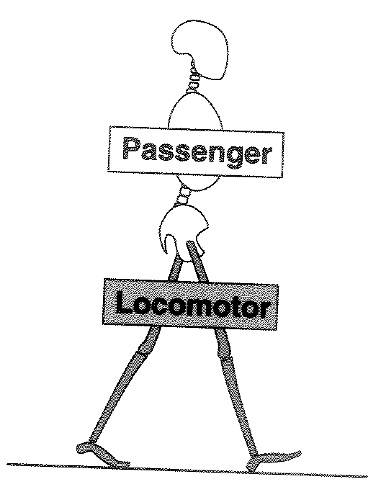
Gait analysis imagines limbs to be an entirely separate unit from the rest of the body. Indeed, Perry's legs seem to walk on their own—at least that's the impression one gets from her textbook:
During walking the body functionally divides itself into two units, passenger and locomotor. While there is motion and muscle action occurring in each, the relative intensity of these functions is markedly different in the two units…. Normal gait mechanics are so efficient that the demands on the passenger unit are reduced to a minimum, making it virtually a passive entity that is carried by the locomotor system. 7
In Perry's description of human walking, the walker is reduced to a mere passenger. All the action is initiated by the legs and hip seat, which seem to have a mind of their own. The passenger is simply going along for the ride. As you can see, Perry's graphics are pared down.
Perry's aim with gait analysis for integrated data systems is to reduce disagreement among observers.
[P]erforming the observation in a systematic manner results in more agreement among observers…The indecisions of subjective observation are avoided. Rapid and subtle events are captured. A printed record of the patient's motion pattern provides a reference base for interpreting EMG, stride and force data. 8
Perry idealizes gait analysis to the extent of suggesting that all subjective indecision among clinicians can be done away with using Gait Lab. If we take her argument to its logical end, then the computerized integrated data set can magically place itself inside the clinician's mind or replace the clinician altogether so that human subjectivity is swept away.
This photograph shows how Gait Lab is set up at the battalion. Photograph taken by author.
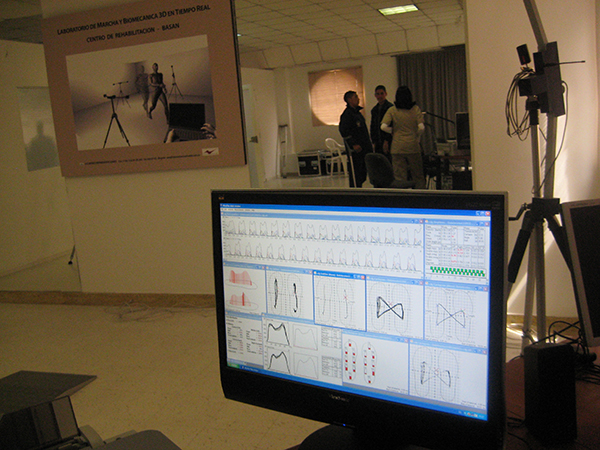
In the poster hanging on the wall on the left, the patient is placed within the 'machine' through a set-up of video cameras, body sensors, and a screen. The clinician, on the other hand, is a computer with a set of hands. The rest of the clinician's body falls out of the frame. This perhaps explains why some physical therapists don't find Gait Lab an exciting venture. For example, when I told Maria at the military hospital that I was observing Gait Lab at the battalion, she responded that she could determine proper gait using her skills as a physical therapist and didn't see what the advantages of Gait Lab were. The orthopedic surgeons nodded in agreement. Not everyone sees the benefits of Gait Lab for the Colombian medical practice, despite Perry's endorsement.
However, Linda did express enthusiasm for learning how to use Gait Lab. She felt it could complement her therapeutic practice and potentially improve the rehabilitation of her patients by providing a more precise evaluation of how patients use their prostheses. Injury caused by prosthesis is commonplace in a rehab unit. In the rehab unit, patients commonly develop large sores. Others will remove their socket liners after practicing to only to find them stained with blood. Injuries that are more serious, still, develop over time. After many years of the prolonged use of a prosthesis, bodies change and patients sometimes develop scoliosis or constant fatigue, creating a more disabling condition than what amputation initially caused. This problem is not isolated to Colombia's national rehabilitation efforts. In recent US history, polio survivors were pushed to walk again and endured strenuous rehabilitation to regain physical strength. Today, post polio syndrome is well documented and has shown that rehabilitation focused on getting people to walk again can produce enduring injury to the body. 9
Linda hoped that through calibration, prosthetic side effects could be reduced. However she explained to me that Gait Lab was difficult to learn. She still had not figured out how to configure the cameras for the computer system. Positioning the cameras and body sensors to the particular height and joint articulations of each patient was especially time consuming and yet necessary for Gait Lab to work properly. Yet Linda remained dedicated to the task because she believed that Gait Lab could capture aspects of a patient's gait cycle that might escape her own observations. She described Gait Lab as getting "what was really wrong with the patient," though when she reflected on Gait Lab as a practice she described it as useless for communicating with clinicians in other Colombian hospitals. "If I send this to a hospital, they will say, "what is this woman talking about?!" While Linda believes the unintelligibility of Gait Lab could be remedied if all hospitals in Colombia eventually learned how to use it, she also recognizes this is more of a dream than a reality.
It's very difficult for other parts of Colombia to have this technology but maybe it could be a dream for the future. It would require financial support, training which is another cost, and all other kinds of reorganization of people so that people in other hospitals could read and know how to use my Gait Lab reports.
She also describes the tedious nature of working with Gait Lab.
We have to sit and look at every millimeter, at every value. It takes some time to place the sensors on the patient's body just right. Since we want the patient to repeat the evaluation throughout his rehabilitation, we have to make sure the patient doesn't turn his head as he walks. [Do you mean he has to walk without any distractions?] He has to walk without distractions so that we can measure a motion pattern. If I were to say, 'hey look' and if he were to turn his head, the pattern changes.
I also have to recalibrate the space of mediation which is that camera over there with the computer system so if the patient is very tall or short I have to move the camera so that we capture everything, all the signals. One time we didn't get an image at all and we all said, "but everything is fine" and then we looked and saw that the patient's trunk was rotated. Since he had a problem with his spine, the sensors didn't come out because we couldn't get the space and the cameras to detect them.
Since Gait Lab work is so tedious, Linda explains that she can only see a few patients in one day. At any given month, 200 or so patients pass through the battalion and military hospital rehabilitation units. Since rehabilitation is a daily practice, many patients don't simply pass through for a check-up. It is clear that seeing 2 or 3 patients in one day doesn't meet the practical needs of the rehabilitation unit. Linda also noted that by focusing on the cameras, sensors and the screen, therapists might ironically forget to look at the patient altogether.
To sit and analyze a patient is hard, and you always have to be there and wonder Why am I doing this? and then look at the data again. What I mean to say is that the technology helps us a lot but at the same time it may cause us to leave aside what we see in him, the patient.
In takes an inordinate amount of time to analyze the massive streams of data that technological analysis yield: the horizon of intelligibility becomes so distant that the patient sometimes escapes the clinician's view. It is hard to know what Gait Lab's future will be in Colombia, but currently its power seems to lie in an imagined future. As we have seen, everyone does not share excitement over Gait Lab. Although Gait Lab may have limited use for clinicians, corporations have invested interest in promoting it. It produces data that prosthetic engineers feel they can use to advance prosthetic design and affect their product line. Meanwhile, physical therapists typically assume the burden of tedious work while being subjected to information overload.
Phantom Limbs and the Strangely Familiar
I now turn to the ways patients talked about their experiences with limb loss, phantom limb sensations, and rehabilitation. I show how, unlike Perry's model, incorporating prostheses into the body is inevitably an intersubjective activity that involves feelings of strangeness and familiarity. If you close your eyes and move your arm up and down, you can vividly feel where your arm is in time and space. However, what if a person loses his or her arm, consciously knows it is missing, and still feels it moving? This is a rather common experience. To describe phantom sensation, Ambroise Paré, a French surgeon from the sixteenth century, suggested an analogy "with the feeling of being pulled by the shirt, where the body is being acted upon, and acts, with reference to an absent or intangible force." 10 Hernan, a young soldier and recent amputee explained to me, "you are lying down and you feel your foot and you go to scratch it and it causes a lot of problems." He felt his phantom limb as a very perturbing sensation — an itch that could not easily be relieved, and he told me he wished the phantom limb would disappear altogether. Many recent amputees made similar comments describing the burning and itching sensations associated with their phantom limbs.
One reason the phantom remains shrouded in mystery has to do with its preferred context of appearance. As one soldier explained it to me, "I feel it at night. It's like the nerves of my toes itch and it's very painful but then some time passes and the pain goes away. When I put on my prosthesis the pain is gone. I feel it at night. At night is when I really feel it." Many patients described how they would suddenly get the urge to use the bathroom in the middle of night and in a half waking state forget that their limb was missing. Sensing their phantom limb they would try to get out of bed and then suddenly fall to the floor. Freddy explained, "I believe one feels your phantom limb for the rest of your life. The massages they [physical therapists] give us have made it start to go away. I feel it less now than I did before. I sometimes go to itch it and I realize it's missing. Once after recently being operated [on] I felt my leg so I started to stand up but I fell." Cesar said, "I would forget that I didn't have my leg and accidentally [try to] put my sock on my missing foot."
The way soldiers talked about their phantom sensations always indexed a lack. Trying to stand on a phantom limb, they would fall to the floor. Forgetting that he had lost a limb, Cesar tries to put a sock on only to find thin air. The blurry border between daytime and nighttime, between sleeping and waking, between memory and forgetting, between an intimate sensation and an artificial apparatus always demonstrated how the intended actions were left wanting. The scratch never satisfies the itch.
Eventually, people typically become more accustomed to their phantom limb sensations and these kinds of problems become less frequent. Nonetheless, amputees frequently discuss how activities once considered 'natural' have become extraordinary tasks. Even as the prosthesis becomes naturalized, depending on circumstance, people may occasionally see them as alien parts—as evidence of something familiar yet, somehow, estranged from the body to which it is attached.
Freud famously described the uncanny, or what he termed the 'unheimlich' (the unhomely) through Hoffman's tale The Sandman. In The Sandman, a father, Coppelius, gives his son, Nathaniel, a spyglass. Nathaniel looks through the spyglass and becomes spellbound when he sees a beautiful automaton Olympia dancing. He falls in love. However, Nathaniel goes mad when suddenly Olympia is pulled apart and disassembled by her makers. (Her makers, understood as paternal figures, are the same ones who constructed Nathaniel's spying glass). Seeing her disassembled, he discovers she is merely an illusion, an inert object appearing human. Clara, a childhood sweetheart he had forgotten in favor of Olympia, then nurses him back to sanity. Nathaniel's mistaken love is taken for amusement among onlookers who felt they could clearly see that Olympia was inanimate, however they are soon disquieted by the memory of Nathaniel's love and become anxious at the thought that they too have mistaken the nature of their beloveds. "A horrible distrust in human figures in general arose," in Hoffman's words. 11
Freud interprets Hoffman's tale as an example of castration anxiety where the father gets in between a man and the object of his desires. Freud hones in on the moment at the end of Hoffman's tale when Nathaniel looks again through the spying glass and catches a glimpse of his father, Coppelius. Nathaniel convulses in a wild frenzy. Freud interprets Nathaniel's nervous attack as the memory of his father's power to take away and destroy what Nathaniel desires. For Freud, the fact that Nathaniel is unable to distinguish what is truly alive from what is mechanical is not primordial, but instead evidences Nathaniel's fear of castration. An alternative reading of Hoffman's tale suggests that Coppelius did not come in between Nathaniel and what he desired, rather what Nathaniel desired was the return of his father. As philosopher Stanley Cavell has pointed out, it is when Nathaniel looks through the spyglass again and sees Clara before him, obstructing a full view of his father, that Nathaniel enters into an excited state. 12
If we accept this latter interpretation, then the uncanny arises from a recognition that the world can be undone; it provokes a desire to return to the world by recreating it. If language and the order of the Law is a paternal figure based in negation (the paternal 'no') as Lacan has suggested, then the uncanny is a problem rooted in a kind of grammar where categorical distinctions are readily blurred. 13 This seemingly primordial anxiety arises from the inability to distinguish the mechanical from the natural, dream life from the waking life, and masculine figures from feminine ones. The human figure and its capacity to repudiate itself incite anxiety. Likewise, the prosthesis has the capacity to repudiate itself — to appear as artifice—as a figuration, or reification, of the 'human.' The prosthesis circulates in a theatre of lack where the signifier "always arrives at its destination": 14 back into the order of prescription. 15
Don Victor, an elderly civilian man, lost his leg many years ago in Antioquia after walking through a minefield on his way to the gold mine where he worked. When we first met, he confessed to having lived, intermittently, in several different shelters, and to being displeased with his prosthesis. In fact one day, in a bout of frustration, he grabbed his prosthetic leg, held it up, and said, "this is not the same thing." By "this," he meant the prosthetic limb did not replace his flesh limb. Or as Stanley Cavell would have it, "[T]he familiar is a product of a sense of the unfamiliar and of the sense of a return means that what returns … is never (just) the same." 16 Don Victor expresses a fundamental difference between a prosthetic limb and his flesh one—the prosthetic limb wears down within a couple years and needs constant repair whereas his former flesh limb did not wear down in this way. He is frustrated because after several years of wear and tear his prosthesis is, literally, falling apart. He desperately needs the clinic to fix his old, tattered prosthetic limb, or give him a new one. He explains that he feels desperate as he could no longer drive a taxi or work the gold mines as he had before. He worried for the economic and emotional well being of his family.
I ask Don Victor if he has ever experienced the sensation of a phantom limb. He responds that he finds phantom limbs to be a common experience among amputees.
Everybody who has lost a leg feels their leg and feels their foot. Yes, I feel it. I always talk about this with other people who have lost limbs. You know you don't have it, but you feel it. You feel that your leg itches. You go and itch your foot and you discover it's the prosthesis. You feel movements. You feel your leg that's true. It's a good thing to feel it. I don't understand it and I will never understand it. I feel my leg whether I have my prosthesis on or off. I'm convinced I don't have my leg. We left it in the minefield….[earlier in the interview, he had described how when he was being rescued by his sons, they had no choice but to leave his amputated limb in the field]. I barely take the prosthesis off. I take it off only to bathe and sleep. I am so accustomed to my prosthesis. I love my prosthesis as if it were my own leg. I have to love it because it helps me a lot to walk. I simply put on my prosthesis and that's it. It doesn't fall off.
For Don Victor, prosthetic walking is now old hat. Aside from occasional itching, his phantom leg does not apparently bother him. He loves his prosthetic limb. And, his enthusiasm is in due in part to the fact that he had only recently obtained a new leg when I met him. Don Victor's discussion of his experience with phantom sensations and prosthesis inspires no metaphysical discussion. "I simply put on my prosthesis and that's it. It doesn't fall off." When Don Victor tells me, "I don't understand it and I will never understand" phantom limb syndrome, I understood him to be highlighting the limits of knowledge. Some philosophers have reached similar conclusions. Soren Kierkegaard, for example, perhaps best captures this insight in suggesting it is a leap of faith that allows a dancer to leap into the air and land in perfect form without second guessing if her body is capable of it. 17
Aesthetic Enhancements
A young soldier and recent amputee Rodrigo described his prosthesis as a toy. In a recorded interview, he recalls:
When I first put on my prosthesis it felt strange but I thought it looked cool because one thinks you still have your foot but you don't so the prosthesis is like a toy but good. It helps you not feel badly. [A toy, how so?] How can I explain this? It's a toy because it is fake. I don't know, but that's how it is.
As much as the prosthesis becomes incorporated into the body's image of itself, it is still widely seen as artifice — an aesthetically pleasing substitute or aid that can help people walk again and feel better about the way they look.
When I first began fieldwork at the military hospital, I sat quietly among a group of soldiers waiting to have their limbs repaired. Perceiving my newness to the hospital scene, some of the soldiers smirked and then pulled off their limbs and used them as elbow rests. By taking the prosthetic off their leg and using it as an armrest, we were all urged to laugh. Treating legs like things is literally found in common speech in the Spanish language. In Spanish, speakers do not generally use possessive pronouns to refer to their body parts. It is more proper to say El brazo me duele ("The arm hurts me") rather than Mi brazo me duele ("My arm hurts me") as one might say in English. However, people will use the possessive pronoun to differentiate their body parts from other people's body parts if there's reason for confusion. I think we all laughed because the soldiers had deliberately confused body parts with objects generally considered to reside outside the body. For prosthetic users who have lost limbs, the doubleness of being and having a body is perhaps made more literal through their use of prosthetic technologies, and hence opens the possibility to play with the boundaries between subjects and objects.
Another day, Wilson, a soldier amputee, told a comical story—one among many funny stories he told at the rehab unit, but one that particularly got patients and therapists roaring with laughter. It consisted of one patient, Ramon, who needed to repair his limb after sustaining a bullet 'wound.' Apparently, someone had assaulted him on the street trying to rob him and when Ramon refused to hand over his money, the assailant shot him in the leg. To the assailant's surprise, Ramon kept walking and did not show evidence of any pain. The assailant ran off in alarm. Stories about odd circumstances that disrupt non-prosthetic users' expectations inspires heartfelt laughter among everyone at the rehab unit. In this instance, the comic story also reveals everyday anxieties about cyborgs and how humans relate to machines. It is not uncommon for soldier amputees to don their prosthesis and laugh saying, "Now I'm Robocop," referring to the 1987 film.
Anthropologist and philosopher Helmuth Plessner writes that laughter is "a loss of self control," and a "break between the person and their body." For Plessner, laughter brings forth "the eccentric position of the human being" where "we are not only our bodies, but we also have our bodies." This distance between the person and the body does not mean that the materiality of the body has been "overcome" but rather that the person has used laughter to call attention to the body's material limits. 18 At times, soldier amputees at the military hospital treated the body as abject—alien and failing. In the quest to obtain a body that appears "complete," more normal and humanlike, they are confronted with the mechanical nature of prosthetic limbs in need of constant repair and tune up. They were humans encrusted with thingness while at the same time trying to act as a 'human person' in the ideal sense—one with all its limbs. In other words, the prosthesis is both the thing that underscored the body's incompleteness and the thing that completes the body.
The body as thing and the body as disfiguration (the person's failing to make ideal bodily figures, or personas, literal)—these are the experiences that inspire reflection and laughter. They are moments where the gap between the body and the person is revealed, especially when they reveal something tragic about oneself or the world. 19 In a similar way, Charlie Chaplin's satire on industrialization, Modern Times, reveals the sorry lot of the factory worker when Chaplin is devoured by a machine and temporarily transformed into a cog. We laugh as he mechanically kicks his leg in rhythm with the turning wheels and we are invited to reflect on the ills of capitalism. Chaplin literally performs an anti-rite of the work routine. Likewise, when the soldiers whip off their limbs to use them as armrests, they perform an anti-rite, momentarily transforming the rehabilitation clinic from a place of medical discipline to a comic theatre.
Manuel, a 35 year old sergeant who has recently completed his rehabilitation process, comes to the hospital wearing his prosthesis. We meet in the rehab unit as he waited to pick up some cosmetic foam he hopes will give a more "natural" shape to his prosthetic leg. He insists that he normally does not wear it:
Right now I don't use foam. For me, the metal bar is more beautiful even though I tell my friends I'm a bionic man as a way to joke. When I need to use my military uniform—that is my camouflage—then I will use the foam so that I can wear boots, so that I can tie the boots around my leg. Tomorrow I will be wearing my other uniform, the number 3 uniform, which is more elegant and so I will not use foam. I will just wear the bar. I have told the technician to make a removable foam for me so I can take it off when I'm in civilian clothes and put it back on for my camouflage uniform and when I wear boots.
Many soldiers described the different uniforms they wore for different occasions. In the Colombian military, each uniform has a number and a specific purpose. Likewise, each medal carries a special meaning and rank. Manuel is very proud when he wears his number 3 uniform as it is reserved for special ceremonies and training. Moreover, the number 3 uniform includes all his medals. Manuel has not worn a military uniform since he had lost his leg five months prior. For Manuel, this is very important because it symbolizes military recognition for his service. With few exceptions, for most soldiers in the Colombian military, losing a limb means losing one's military status and job. While Manuel is a sergeant, most rank and file soldiers, referred to as suboficiales in the Colombian military, were once farmers or miners for whom entrance into the military represented an elevation in status. Many soldiers explain to me that they want to wear boots with their prosthesis, even though the added weight makes it difficult to walk. In sum, the necessity to walk and incorporate a prosthesis into one's body is not simply about getting around in the world. It carries its own cultural significance—and challenges.
Conclusion: The boundaries of the body
Shaping the boundaries of the body is a work in 'progress' of the political, social and moral kind. In a Colombian medical rehabilitation unit, people incorporate prosthesis into their bodies as a means to achieve full human capacity as defined by the State Medical Board, medical staff, policy makers, corporations, and prosthetic users themselves. In this way, rehabilitation is not a curing science, but a practice in physical, moral, and aesthetic enhancement. I started my essay by showing how prosthetic objects are similar to language in that their apprehension involves skill and personalized style that is learned through ritualized daily practice. 20 With time, their apprehension often becomes "second nature": little effort is required to perform this skill as in the daily activities of walking and speech.
With this essay, I bring to the fore feelings of ambivalence expressed among medical practitioners and amputees towards prosthesis and the increasing technical enhancement of prosthetic walking in Colombia. Medical practitioners express ambivalence towards the mechanization of their practice. They often convey their desire for more sophisticated technologies like those reportedly used in US hospitals to treat veterans returning from Iraq. At the same time, they fear they are being de-skilled by new simulation technologies and cast doubts on the imagined future of telemedicine. The desire to rehabilitate full human capacity attends to different scales of value that are economic, political, and aesthetic. In Colombia, medical practitioners, corporations, and state representatives invest incredible energy in getting a large and growing population of injured men to walk bipedally on prostheses, even when prostheses injure their patients. In some ways, the impulse to prostheticize the war wounded is an attempt to displace the enduring effects of military conflict, to shift it away from the immediate awareness of people who nonetheless live through continual warfare. At the same time, the prosthesis underscores the continual dismemberment of people. Simulation technologies, like those that Gait Lab promotes, reduce walking to numbers and displacing what causes the injury—the reason for the prosthesis, in the first place—and fixing the amputees aspirations on a distant horizon of possibility.
Incorporating prosthesis into the body is not simply about improving mobility, rather its value also lies in aesthetics and artistry. At times amputees aimed to appear naturally 'human,' at other times people preferred to call attention to the mechanical nature of their prosthetic limbs. People did not only use their prosthesis to walk, but also to joke, play, and enhance their style of dress. Medical staff and corporate representatives will routinely refer to prosthesis as "replacement technologies." However, in practice, prosthetic limbs are not mere replacements. People don't merely snap on a prosthesis. Instead, prosthetic incorporations require daily practice. As Jhon Luis, Don Victor and others have noted, people often experience an oscillation between a seemingly natural relations to their prostheses and feelings of 'strangeness' or loss. This strangeness can be described as uncanny, or, as Stanley Cavell puts it, the "recognition of an uncertainty in our ability to distinguish the animate from the inanimate." This uncertainty allows people to deny something they find frightening. People may feel anxious and wonder if by 'animating' and incorporating mechanical parts into their bodies, they have given up their status as full human persons. The prosthesis may also serve as a reminder of what most people may prefer to forget—their own dismemberment.
I'd like to thank Emily Martin, Julie Elman, and Kathryn Chetkovich for reading drafts of this essay and providing their comments. I'd also like to thank Michael Ralph and Brenda Brueggemann for their editorial work. I presented versions of this essay at the Medical Anthropology Association Meeting at Yale University, the NYU Science Seminar, the Limits of Memory Conference at the New School, and the Worn Bodies workshop at Lancaster University. I'd like to thank participants who provided me provocative challenges and comments to the work I presented. I'd especially like to acknowledge Lesley Sharp, Lucy Suchman, Deborah Steinberg, Gillian Einstein, Esra Ozcan, and Michalis Kontopodis for their comments and words of encouragement during these presentations. Lastly, I'd like to extend my thanks to Michael Ralph, who kindly invited me to submit this essay. The National Science Foundation, the Wenner-Gren Foundation, the NYU Torch Fellowship, Fulbright Colombia, and the ACLS financially supported the research and writing of this project.
- Bruno, R. (2003). The polio paradox. Clayton: Warner Books.
- Buck-Morss, S., & Benjamin, W. (1989). The dialectics of seeing : Walter Benjamin and the Arcades project. Cambridge, Mass.: MIT Press
- Cavell, S. (1988). In quest of the ordinary : Lines of skepticism and romanticism. Chicago: University of Chicago Press.
- Critchley, S. (2002). On humour. London ; New York: Routledge.
- French, L. (1994). The political economy of injury and compassion: Amputees on the Thai-Cambodia border. In T. J. Csordas (Ed.), Embodiment and Experience. Cambridge: Cambridge University Press.
- Grosz, E. A. (1994). Volatile bodies : Toward a corporeal feminism. Bloomington: Indiana University Press.
- Kierkegaard, S. (1954). Fear and trembling, and The sickness unto death. Garden City, N.Y.,: Doubleday.
- Kurzman, S. (2002). "There's no language for this": Communication and alignment in contemporary prosthetics. In K. Ott, D. Serlin & S. Mihm (Eds.), Artificial parts, practical lives: Modern histories of prosthetics (pp. 227-248). New York: New York University Press.
- Lacan, J. (1972). Seminar on "The Purloined Letter". Yale French Studies, 48, 33.
- Llinas, R. (2003). El cerebro y el mito del yo. Bogota: Grupo Editorial Norma.
- Martin, E. (1987). The woman in the body : A cultural analysis of reproduction : With a new introduction ([2001 ed.). Boston: Beacon Press.
- Martin, E. (1994). Flexible bodies : Tracking immunity in American culture : from the days of polio to the age of AIDS. Boston: Beacon Press.
- Mauss, M. (1985). A category of the human mind: The notion of person; the notion of self. In M. Carithers, S. Collins & S. Lukes (Eds.), The category of the person: Anthropology, philosophy, and history (pp. 1-25). Cambridge: Cambridge University Press.
- Mauss, M. (1992). Techniques of the body. In J. Crary & S. Kwinter (Eds.), Incorporations. New York: Zone
- Mitchell, S. W. (1872). Injuries of nerves and their consequences. Philadelphia: J.B. Lippincott & Co.
- Perry, J. (1992). Gait analysis: Normal and pathological function. New York: McGraw-Hill, Inc.
- Plessner, H. (1970). Laughing and crying: A study on the limits of human behaviour (J. S. Churchill & M. Grene, Trans.). Evanston: Northwestern University Press.
- Ramachandran, V. S., & Blakeslee, S. (1998). Phantoms in the brain : Probing the mysteries of the human mind (1st ed.). New York: William Morrow.
Endnotes
-
(Mauss, 1985)
Return to Text -
For more on La Violencia and concepts of bodily dismemberment, see (Uribe, 2004)
Return to Text -
(Mitchell, 1872)
Return to Text -
(Llinas, 2003)
Return to Text -
(Ramachandran & Blakeslee, 1998)
Return to Text -
(Martin, 1994)
Return to Text -
(Perry, 1992)
Return to Text -
(Perry, 1992)
Return to Text -
(Bruno, 2003)
Return to Text -
(Grosz, 1994)
Return to Text -
Hoffman as quoted by (Cavell, 1988)
Return to Text -
(Cavell, 1988)
Return to Text -
(Lacan, 1972)
Return to Text -
(Lacan, 1972)
Return to Text -
Cavell writes, "The return of what we accept as the world will then present itself as a return of the familiar, which is to say, exactly under the concept of what Freud names the uncanny. That the familiar is a product of a sense of the unfamiliar and of the sense of a return means that what returns after skepticism is never (just) the same." (Cavell, 1988)
Return to Text -
(Cavell, 1988)
Return to Text -
(Kierkegaard, 1954)
Return to Text -
(Critchley, 2002; Plessner, 1970)
Return to Text -
(Critchley, 2002)
Return to Text -
(Mauss, 1992)
Return to Text

